The Kenyan Ministry of Health has unveiled a comprehensive five-year plan to tackle tuberculosis (TB), leprosy, and lung diseases.
Dubbed the “National Strategic Plan for Tuberculosis, Leprosy, and Lung Health” (2024–2028), the initiative aims to ensure equitable access to quality care for all Kenyans suffering from these preventable conditions.
The plan aims to address cases of misdiagnosis, which have led to preventable deaths. In addition, the plan represents a significant step toward a TB-free Kenya by prioritizing quality care, accurate diagnosis, and community engagement
Principal Secretary for Public Health and Professional Standards Mary Muthoni expressed concern about rising TB cases, with 90,560 reported in 2022 compared to 77,854 in 2021.
“Alarming as this figure is, it represents only 68% of the estimated 133,000 TB cases that were likely to emerge that year, leaving 32% undiagnosed and untreated. The emergence of drug-resistant TB cases, totalling 756 in the same period, highlights the urgent need for a comprehensive and coordinated response,” the PS said.
Data from the National Tuberculosis, Leprosy, and Lung Disease Programme (NTLLDP) in November 2023 shows encouraging progress, with 90,841 TB cases identified out of an estimated 112,000, compared to a significant drop in 2020.
The number of drug-resistant TB cases has also decreased, from 957 in 2020 to 756 in 2023.
“The strategic plan, therefore, becomes a vital advocacy tool for resource mobilization across all sectors, including the private sector. It encourages innovative financing to meet the needs of the people, and I call upon all stakeholders to join hands in this endeavour,” she noted.
New Guidelines to Manage Tuberculosis and Asthma Launched in Kenya
Drivers of TB in Kenya
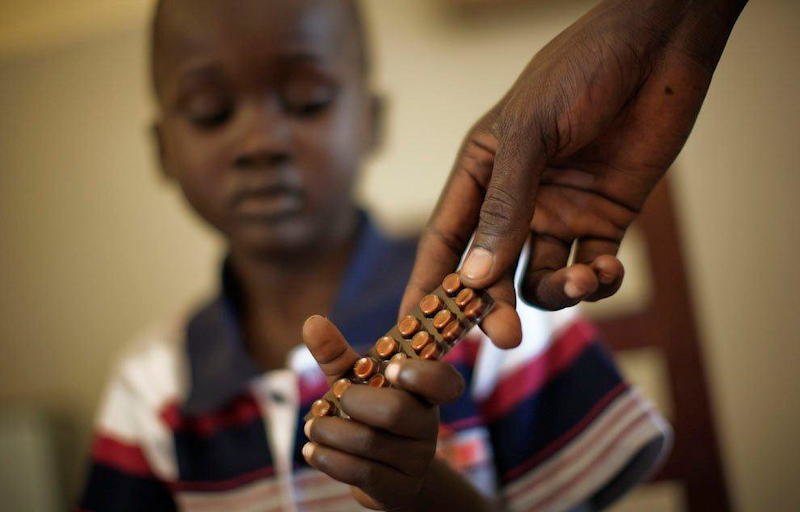
Poverty, undernutrition, HIV infection, alcohol use disorders, smoking, and diabetes mellitus are the key social determinants of tuberculosis (TB) in Kenya.
These factors contribute to the high prevalence of TB in the country, making it one of the top 30 high-burden TB/HIV countries globally.
Poverty
Poverty is a major risk factor for TB, as it can lead to overcrowding, malnutrition, and poor access to healthcare. In 2022, 17% of Kenyans lived on less than USD 1.90 per day, placing more than 8.9 million Kenyans in extreme poverty. This situation is particularly dire in rural areas, where 7.8 million people are living in extreme poverty, compared to 1.1 million in urban areas.
Undernutrition
Undernutrition is another major risk factor for TB. A Kenya population-based HIV impact assessment (KENPHIA) survey conducted in 2018 estimated the burden of undernutrition in Kenya to be 24.8% in 2018.
This malnutrition is particularly prevalent among children, with 4.2% suffering from wasting and 19.4% experiencing stunting.
HIV Infection
HIV infection is a major co-morbidity with TB, with WHO estimating an incidence of 35,000 people with TB and HIV co-morbidity in Kenya in 2020.
This co-infection is particularly deadly, with WHO estimating that 12,000 people succumbed to the co-infection in 2020.
Alcohol Use Disorders
Alcohol use disorders are also a major risk factor for TB, with 11% of Kenyans deemed heavy episodic alcohol consumers. Alcohol weakens the immune system, making people more susceptible to infection.
Smoking
Smoking is another major risk factor for TB, with the same percentage of the population smoking tobacco as those who engage in heavy episodic alcohol consumption.
Smoking damages the lungs and airways, making it easier for TB bacteria to take hold.
Diabetes Mellitus
Diabetes mellitus is a rapidly growing risk factor for TB in Kenya, with the International Diabetes Federation projecting a rapid increase in the number of people with diabetes mellitus (DM) from 190,000 in 2000 to 1,965,000 in 2045.
Diagnosis rates for DM are low, with two-thirds of the estimated number of people with the condition unaware that they do.
UN Report Warns of Big Misses Across Sustainable Development Goals